ARTICLES
Ethics in occupational health and safety: case studies from Gujarat
Jagdish Patel, Siddarth David
DOI: https://doi.org/10.20529/IJME.2016.060
Abstract
Rapid industrialisation in India is giving employment to millions of people in the formal sector, and many more in the unorganised sector. However, the absence of clear policies, poorly enforced regulations, lack of systematic reporting of occupational diseases, lamentable socioeconomic conditions of the workers and their limited access to healthcare make occupational health and safety (OHS) a critical area.
OHS has received limited attention in mainstream research and policy-making, and remains an issue concerning workers’ groups. Ethical guidelines have not been formulated in the Indian context, though international norms and guidelines exist in the practice of OHS.
This paper considers cases from the heavily industrialised state of Gujarat to elucidate the ethical challenges in OHS and emphasise the need for improving the existing laws. It advocates the formulation of guidelines for ethics in OHS to ensure workers’ health and safety.
Introduction
Barring a few advocacy groups and non-governmental organisations, occupational health in India, especially in the most hazardous industries, has received limited attention in public health policy or mainstream medical research. Consequently, basic occupational health services are scarcely available. Given that ethical issues in health are not taken very seriously, the ethics of occupational health and safety (OHS) is hardly discussed. Since India does not have a strong legal framework for enforcing OHS, it would be useful to examine the existing global ethical codes and guidelines to evaluate the current practices, identify gaps and improve practices in occupational health.
India annually employs a few million people in the formal industrial sector and millions more in the unorganised sector. However, the absence of clear policies, poorly enforced regulations, lack of systematic reporting of occupational diseases, largely unorganised nature of labour, lamentable socioeconomic conditions of the workers and their limited access to healthcare make it imperative to urgently review the status of OHS in terms of research, practice and policy.
This paper presents experiences from Gujarat and elaborates on the violation of medical ethics in the provision of occupational healthcare. The arguments draw upon case studies from one of India’s most industrialised states and focus on violations of the right to information on hazards and confidentiality. The quality of care provided by the Employees’ State Insurance Corporation (ESIC), the fate of medical documents and diagnosis of occupational diseases are also discussed.
Concept of occupational health
In 1995, the Twelfth Session of the Joint International Labor Organization and the World Health Organization Committee on Occupational Health agreed on key principles (previously agreed in 1950) of occupational health. These focus on the maintenance and promotion of workers’ health, improving their working environment, as well as creating a system of support and productivity (1). Over the years, many guidelines and protocols have put these principles into practice. For example, the International Commission on Occupational Health (ICOH) has developed the International Code of Ethics for Occupational Health Professionals, of which India is a member. The code describes the duties and obligations of occupational health professionals and the conditions for the execution of their functions (2). However, in spite of these codes the health condition of workers, safety of their working environments and fulfilment of obligations to them remain far from satisfactory across the globe (3, 4, 5).
Status of legal protection to workers in different sectors
Organised labour, which gets legal protection, comprises about 7% of India’s workforce (6). Legislations for safeguard of OHS mainly concern dock workers and workers in manufacturing, construction and mining sectors. Certain legal provisions, eg the Factories Act, 1948, stipulate that units employing less than 10 workers need not be registered; thus, many workers have no protection (7). Poor enforcement of law leaves many units unregistered and out of the reach of enforcement agencies. Included among this 7% of the workforce are public sector workers in education, health, banking and insurance, administration, etc, who also have no legal provisions for the protection of health and safety at work.
A major sector like agriculture which employs 54.6% of the total workforce has no laws to ensure OHS (8, 9). Each year, large numbers of agricultural workers die or are maimed due to exposure to toxic chemicals, extreme weather conditions, snakebite or machine-related accidents, making it one of the most hazardous sectors to work in (9, 10, 11, 12).
Compliance with international labour laws
India is a founding member of the ILO, but has ratified only 36 of the 177 technical conventions related to health (13). India is yet to ratify three fundamental conventions on OHS, ie the Occupational and Safety Convention (1981) and its protocols (2002), the Convention on Occupational Services (1985) and the Promotional Framework of the Occupational Health and Safety Convention (14).
The impact of liberalisation
A major factor that spurred on the adoption and implementation of major OHS guidelines in India was the process of economic liberalisation introduced in the 1990s. The industrial sector was largely freed from “Inspector Raj”, under which state-appointed inspectors in-charge of enforcing laws would visit the units and allegedly harass owners to pay bribes. The appointment of inspectors was stopped, circulars stating, “Do not visit the unit unless there is a complaint” were issued and self-certification schemes were designed for industries. This policy has been expanded under the present government’s policy of “Ease of doing business”.
Enforcement of laws such as the Contract Labour (Regulation and Abolition) Act (1970), which provided safeguards against employing contract workers were weakened. (15). This led to a surge in the number of contract workers with little access to OHS. A recent survey has shown a rise of nearly 40% in the proportion of contract workers compared to regular workers. The former are paid less than the latter for performing similar tasks and have virtually no job security or benefits, such as medical aid and health insurance (16). Another factor that has weakened the workers’ cause is the decline of trade unions, which have traditionally been the strongest advocates of workers’ rights and the enforcement of OHS norms. Barring construction workers, workers in no other economic sector have been provided legislative cover for OHS since economic liberalisation began.
Key laws, policies and work on OHS
-
The Factories Act, 1948
-
The Employees’ State Insurance Act, 1948
-
National policy on OHS
-
Work by the National Human Rights Commission
One of the first Acts in independent India to protect workers’ rights and ensure their safety, the Factories Act was last amended in 1987 after the 1984 Bhopal gas tragedy. The amended Act stipulates the permissible limits for nearly 120 substances handled at work; however, since then this list has not been reviewed or expanded to include other materials. Also, most of the provisions for monitoring of the workplace environment have not been enforced and the state administrations have hardly brought any prosecutions for the violation of these provisions. Though prosecutions filed under the Factories Act are criminal in nature, in practice, many are settled by Lok Adalats1 (17). Since Lok Adalats are not empowered to deal with criminal complaints, they dispose of matters related to OHS by merely imposing nominal fines.
The Act does not provide for the “right to refuse” work which may pose a danger to a worker’s life and health, it only gives workers the right to file a complaint before the factory inspector for further action, if there is “imminent danger”. Moreover, it does not give workers, trade unions or civil society organisations the power to prosecute in case of any violation. Unless workers and their representatives have the right to prosecute and receive a part of the fine imposed, it will be practically and economically difficult for them to challenge violations of the Act’s provisions.
The Act mentions only 29 notifiable occupational diseases2, with no mention of musculoskeletal disorders. According to the ILO, these disorders are the “single biggest reason for economic losses” (18). In view of this, the Second Labour Commission recommended, in 2002, the enactment of a separate law for OHS and the establishment of a National OHS Commission and OHS Boards at the state level (19). However, this has not been implemented even after more than a decade.
The Employees’ State Insurance (ESI) Act was an important attempt to provide social security to workers, entitling registered employees to medical treatment (20). Workers insured under the Act are also entitled to various benefits, including medical, sickness and disablement benefits. However, the Act applies only to specific geographical areas and sectors. As of March 2014, only 19.5 million workers were covered under the Act (21). Also, in most states, the manufacturing sector includes only those units which have 10 or more employees. While the ESI Act offers various benefits, it does not provide for life insurance (22).
Industries are reluctant to expand the coverage of workers and ailments since this would mean an increase in the employers’ contribution to the funding of treatment. For example, in the Anand district in Gujarat, the government had issued a notification in 2004 for workers in the Vallabh Vidyanagar industrial area to be covered under the ESI Act but the Industrial Association protested and refused to get registration under ESI Act. Instead, they signed a memorandum of understanding with a neighboring teaching hospital to provide medical services to the workers. Though the workers do not have to contribute to the scheme, it does not have many of the benefits covered under the ESI Act, leaving the workers at a disadvantage (22). Also, industrial units, in violation of the provisions of the ESI Act, do not cover all workers, particularly contract workers, badli workers (temporarily appointed to fill in for absent permanent workers) and casual workers, who often perform the most risky jobs. This violates the safeguards provided by the ESI Act. Many new industrial units in Gujarat are not covered under the ESI Act. The situation is likely to be the same across the country.
The Act has hardly helped in the diagnosis of and compensation to workers suffering from occupational diseases. Between 1997 and 2009, the ESI Corporation diagnosed 1576 cases of occupational diseases – an abysmally low figure, given the large number of workers around 19.5 million, employed by the various industries (23, 24).
There is barely any recording of data, which is important for determining the occupational disease burden. An example is that of byssinosis, one of the most common ailments found among workers in the textile industry, a key industry in India. Not a single case was diagnosed under the ESI Act till 1996 and it was only after immense pressure from workers’ groups that such cases were recorded and compensation provided (25, 26).
In 2009, the Government of India notified the National Policy on Health, Safety and Environment at Work. This aimed to reduce the morbidity and mortality from accidents, improve the coverage of work-related injuries and diseases, create a database of such cases, and enhance the monitoring of and compliance with guidelines (27). The policy recognises the importance of workers’ safety and health and regards prevention as vital to the promotion of these. The policy also recommends a review of the national polices and guidelines at least every five years, and seeks to amend the laws relating to OHS to harmonise them with international standards.
The most significant work on OHS has been done by the National Human Rights Commission (NHRC) of India. In a special report submitted to Parliament, it made recommendations on the prevention of and compensation for silicosis (28). In 2006, together with a workers’ rights group, it filed a public interest litigation on silicosis before the Supreme Court. In keeping with the Court’s directions in May 2009, the Commission recommended that the families of diseased workers filing complaints be paid relief of INR 300,000–500,000 (28). States such as Rajasthan (29, 30) have implemented the NHRC’s recommendations and not only pay relief to affected workers, but have also put in place systems for the diagnosis and prevention of silicosis.
Gaps in data
Some data are available on occupational injuries and fatalities, but there are almost none on occupational diseases. For example, there is no comprehensive data on the prevalence of occupational diseases in the mining industry. This is primarily due to the lack of proper surveillance procedures and a comprehensive surveillance programme for occupational diseases (26). Moreover, the available data are not entirely reliable. In 1975, the Labour Ministry constituted a small working group to simplify and rationalise the registers and reports prescribed under various labour laws. Another committee was constituted in 1981 to look into the procedures followed for compiling primary OHS statistics. Many important recommendations made by these bodies and other commissions remain unimplemented (31). Table 1 shows that only 111 cases of pneumoconiosis and 123 of silicosis were detected from 1994 to 2011 (32).
| Table 1: Cases of pneumoconiosis and silicosis (1994–2011) | ||
| Year | Coal workers’ pneumoconiosis | Silicosis |
| 1994 | 07 | 0 |
| 1995 | 05 | 1 |
| 1996 | 16 | 5 |
| 1997 | 05 | 0 |
| 1998 | 02 | 2 |
| 1999 | 03 | 0 |
| 2000 | 06 | 58* |
| 2001 | 00 | 1 |
| 2002 | 03 | 5 |
| 2003 | 05 | 5 |
| 2004 | 34 | 9 |
| 2005 | 08 | 33 |
| 2006 | 04 | 00 |
| 2007 | 08 | 00 |
| 2008 | 01 | 03 |
| 2009 | 0 | 0 |
| 2010 | 1 | 0 |
| 2011 | 3 | 1 |
| Total | 111 | 123 |
| (Source: Ministry of Labour and Employment, Government of India, 2011) | ||
Table1 shows that a significant number of persons employed in the mines may be suffering from occupational diseases. Studies show that in countries without strong notification and identification systems, the prevalence of occupational hazards is far greater than that reported, because in most cases they are not notified (33). Thus, the existing data hardly give a complete picture of the occupational health status of Indian workers.
OHS in Gujarat
Being a major industrial zone and a hub for the manufacturing sector, Gujarat attracts migrant labour from other parts of India. RK Manvar of the Occupational Health and Safety Association filed a right to information application on OHS in three power plants in Gujarat from 2006–2011 and just 109 cases of occupational diseases were found. Following a similar application filed by Shailendrasinh Jadeja, Seva Foundation, Rajkot, it was found that just 12 cases of occupational diseases had been reported officially in eight units in the last five years. This highlights the need for stringent and transparent mechanisms to monitor and report occupational diseases.
| Table 2: Fatal and non-fatal accidents in factories in Gujarat (2011–2014) | ||||
| Year | 2011 | 2012 | 2013 | 2014 |
| No. of registered factories | 37546 | 39181 | 40910 | 42065 |
| No. of non-fatal accidents | 3014 | 2781 | 2285 | 1751 |
| No. of fatal accidents | 249 | 216 | 218 | 249 |
| No. of fatalities | 249 | 216 | 229 | 259 |
| (Source: Directorate General, Factory Advice and Labour Institutes, India, and Director of Industrial Safety and Health, Gujarat) | ||||
Table 2 shows that in Gujarat the number of occupational injuries has fallen drastically, while that of fatal occupational accidents remains unchanged (34, 35). Studies show that near miss accidents, lost-time accidents, serious injury accidents and fatal accidents form a pyramid, with near-miss accidents at the bottom and fatal ones at the top. Thus, to reduce fatal accidents one must reduce near-miss accidents, and fatal accidents would be reduced in proportion to the reduction in the other types of accidents (36).The situation in Gujarat seems unusual, considering that the number of non-fatal accidents has decreased but that of fatal accidents has risen. A possible explanation could be that the number of injuries is highly under-reported. This would be true of the rest of India as well.
After the revision of salaries by the 6th Pay Commission, government employees’ salaries increased substantially and individual states could not cope with the added economic burden. Consequently, there has been a reduction in the number of government employees, including factory inspectors. Data show that nearly a quarter of the 972 sanctioned posts of factory inspector are vacant (34). There is great variation between different states and Union Territories, eg nearly half the posts of factory inspector are vacant in industrialised states such as Punjab, Maharashtra and West Bengal, while almost two-thirds are vacant in underdeveloped states such as Bihar and Chhattisgarh. One-third of these posts are vacant in Gujarat. The only post of industrial hygienist, which has been filled, has been sanctioned in Rajasthan (34). With the increasing number of factories and workers, it is essential to increase the number of factory inspectors to ensure compliance with the norms and reporting of accidents. It is possible that fewer inspectors would mean the reporting of fewer injuries. In the course of his work in Gujarat, the first author got the impression that limiting the number of factory inspectors could be a means by which the state and industry deliberately under-report industrial accidents.
Ethics of OHS
Globalisation and the increased demand for industrial production have made it necessary to address the ethical dilemmas faced in the practice of OHS (37). As the ethical aspects of this area have not been fully formulated, there is limited scope for enforcement, especially in low- and middle-income countries (LMICs), which have weak regulatory frameworks. In such cases, international guidelines are the only parameters for dealing with ethical challenges and measuring the gaps in the practice of OHS (33). In the absence of strong legal systems of enforcement, the development and institutionalisation of ethical codes and guidelines would effectively enhance ethical practice (33). This necessitates an examination of the ground realities through the lens of such codes or guidelines.
The ICOH (2) developed codes of ethics on the basis of the experiences of LMICs. It listed principles, conditions for following them and duties for putting them into practice (Figure1).
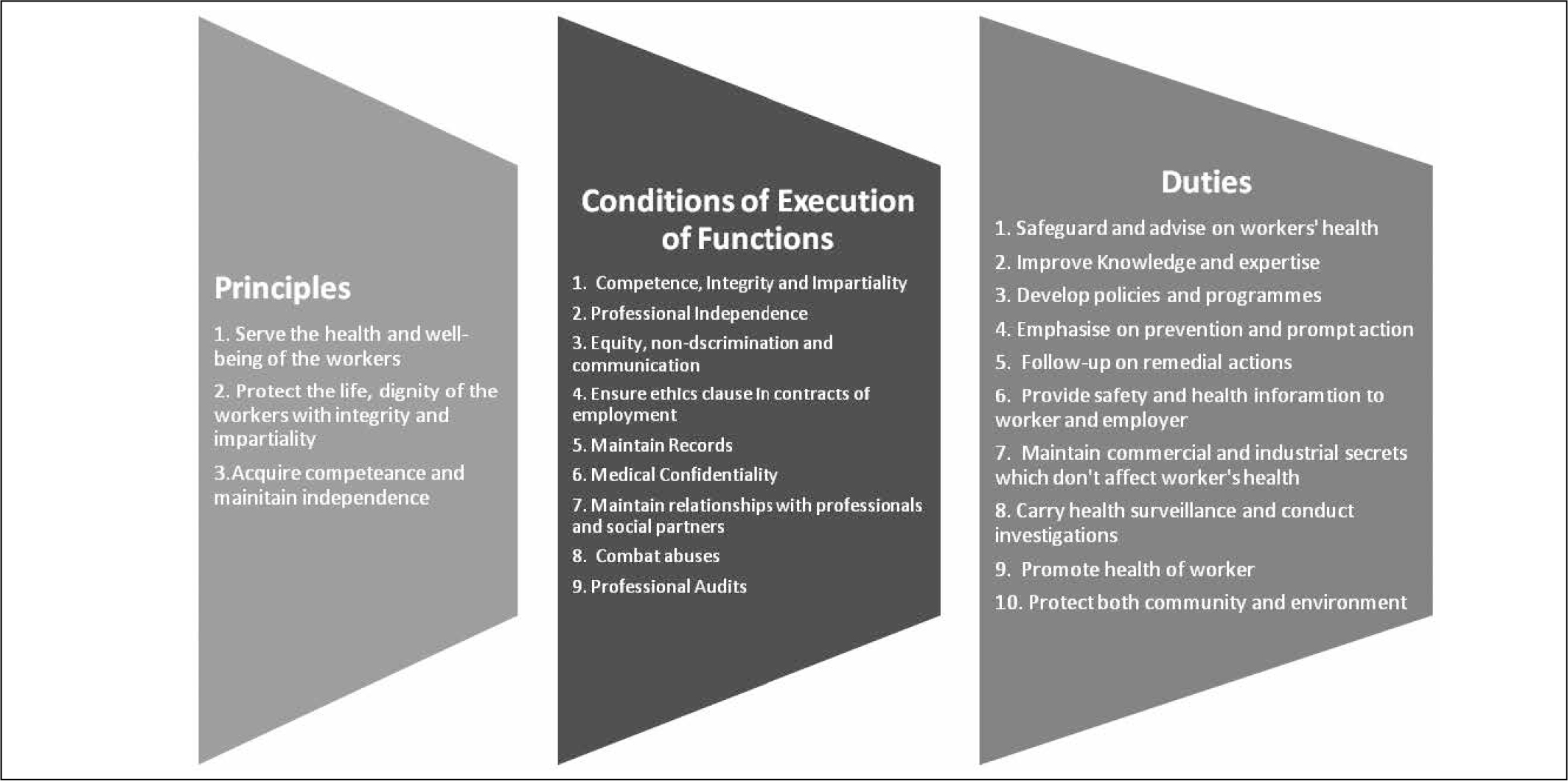
The codes stress that while the primary goal of occupational health is to prevent work-related diseases, this cannot be done without protecting and maintaining the workers’ overall well-being. They address occupational health from the perspective of human rights and social requirements. With their holistic approach, the codes emphasise prevention, cure and rehabilitation (2: p3). They also highlight occupational health providers’ duties, such as adopting a non-discriminatory approach, providing workers with information on health risks and auditing their own services (2: p10). Thus, they can serve as a comprehensive framework to assess the state of occupational health services.
The paper will now discuss the ethical challenges in OHS, using case studies collected by the first author during his interaction with workers and worker advocacy groups in Gujarat3. These will be explored in the light of the ICOH Codes.
Case 1
In a coal-based thermal power plant, a worker concerned about the dense clouds of coal dust went to the medical officer and inquired about the health consequences of inhaling the “black smoke”. The doctor assured him that the smoke was quite harmless and would be passed out of the body with urine. Given the ample evidence of serious damage to the alveoli due to the inhalation of fine dust particles and critical health risks such as coal miner’s pneumoconiosis, the occupational health professional grievously violated his duty to communicate health risks.
Providing information on health risks is crucial for the prevention of disease, as well as motivating workers to undergo regular medical check-ups. Often, however, medical officers appointed by the factory management fail to give correct and timely information. This is a blatant violation of occupational health ethics. In a related case, a woman worker exposed to the fine dust of polyacrylate was suffering from respiratory problems and approached the medical officer, who referred her to a government tuberculosis centre. An X-ray was performed and the radiologist’s opinion recorded, but nowhere was her occupational history noted. Her test results did not tally with a diagnosis of tuberculosis, yet she was put on anti-tuberculosis treatment and died a few months later. There are instances in which workers exposed to different types of dust particles approach doctors and are routinely put on anti-tuberculosis treatment, even if the smear is negative. This points to deliberate malevolence or ignorance on the part of the doctors and occupational health professionals. Both possibilities are violations of occupational health ethics.
Case 2
A worker in a paracetamol manufacturing unit approached us for guidance. He was suffering from skin rashes, which we suspected from his history were occupational in origin. We consulted a dermatologist practising privately for a patch test, before approaching the ESIS. This dermatologist got the worker to provide samples of chemicals handled by him and carried out patch tests for all of them, including caustic lye, and informed the worker that he had occupational dermatitis. The caustic lye burned the skin, causing the worker immense pain. The doctor admitted that he did not know the concentration which had to be used for such tests and had used it undiluted. Finally, he refused to certify it as a case of occupational dermatitis as he had been guilty of an unethical practice during testing.
This case highlights the need for occupational health workers to not only maintain and provide written records, but more importantly, uphold their integrity. Providing written records prevents partiality and reduces the chances of tampering.
Case 3
An ESI hospital launched a full body check-up service for the units in the city. They were requested to send their workers for a check-up during a specified time period. Some workers complained that they were not being given the reports of the examinations. When the ESI authorities were approached, they said reports are confidential and cannot be given to the workers. According to them, the factory managements were their clients, not the workers. When reminded that the workers contributed to the ESI from their wages, and when told that they were the clients since these were their own health reports, the ESI authorities started giving the workers the reports, but shared them with the factory management.
Occupational health professionals should respect and maintain the confidentiality of the health records of the workers. Providing their reports to the management without their consent or knowledge is a violation of confidentiality. The author came across other instances in which factories appointed medical officers and regular check-ups were carried out, but the reports were made available only to the managements. Even when they were made available to the workers, they were not explained to them. What is the purpose of reports whose significance is not made known to those who require them the most?
The management often arranges for private treatment for workers injured in workplace accidents at a clinic or hospital. When the workers ask the doctor for the treatment papers, the doctor refuses on the ground that the cost of the treatment was borne by the management. In such circumstances, it becomes difficult for the worker to get follow-up care and file for rehabilitation claims. This raises the question of who owns the case papers: the patient or the management? If the person who pays for the tests owns the reports rather than the patient, does it not compromise the latter’s confidentiality?
Case 4
A worker exposed to chromium compounds in a manufacturing unit visited the local ESI dispensary for ulcers on the foot, most probably chrome ulcers. The medical officer neither examined the ulcer, nor asked for his occupational history. She simply handed him a prescription. Later, when she discovered that the worker was accompanied by an occupational health activist, she hastily took the prescription back and tore it up. She then followed the standard procedure of referring the patient to the ESI dermatologist. The latter did not examine the worker’s foot or take his history. He straight away wrote a prescription. On becoming aware of the activist’s presence, he took the prescription back and said that a patch test was required to confirm the diagnosis and ascertain if it was an occupational problem. For the test, the worker himself would have to provide a sample of the chemicals from the factory. The worker said this would be difficult. The matter ended there.
In another case, a worker visited the same skin specialist. He was accompanied by the same activist, who introduced himself as a safety officer of the factory where the patient worked. The doctor was very polite this time and followed the due procedure.
This change in demeanour and compliance with the norms in the presence of a factory officer indicate where the loyalties of occupational health professionals lie. They have no sense of responsibility towards the workers, whose health is supposed to be their primary concern. If their behaviour is dictated by the presence of a factory officer, what becomes of the principles of impartiality and non-discrimination?
Case 5
The author followed up the cases of some workers who were suspected to have silicosis and had been admitted in a general hospital. They were discharged before the diagnosis was confirmed. Due to their deteriorating health, they returned to the hospital, where they were sent to the tuberculosis ward. The examining doctor wrote “referred to NIOH” in English and the workers were told to go to a “hospital” in Ahmedabad. The author told the doctor that the National Institute of Occupational Health (NIOH) can be consulted only before referral. Moreover, the workers were unable to travel to Ahmedabad, either due to ill health or shortage of money. However, the hospital refused to admit or treat them. They were finally admitted following the intervention of the State Health Commissioner (SHC).
Later, the doctor who had examined the workers wrote to the SHC that the diagnosis could not be made because the hospital did not have a CT scan facility. The standard protocols on the diagnosis of silicosis require only a chest X-ray and the patient’s occupational history. The author then sent the relevant portions of standard medical textbooks to the doctor, who was furious. Next, he confided in the author that he felt a sense of pressure from the state government not to diagnose silicosis, and that he feared losing his job if he did so. When advised to respect ethics rather than succumb to pressure, he refused.
Occupational health professionals face strong external pressures from the powerful industrial and political lobbies, which would rather avoid paying compensation to workers. These pressures affect their professional independence and impartiality. Only institutionalisation of ethics in occupational health can help mitigate such pressures.
Case 6
The author visited a chromium factory when an NIOH team arrived from Ahmedabad to carry out investigations and collect samples, following numerous news reports about workers with nasal septum perforations and dermatitis. The author and workers sought to know more about the study’s objectives and the team’s plan and asked for the results to be shared with the workers. The team agreed, and collected samples of blood, urine and semen. For the collection of the semen samples, the male workers were asked to masturbate in a corner, with no regard for privacy. Since there was no word from the team even months later, the author made enquiries with the NIOH. He was informed that the report was being prepared. A few months later, the NIOH said it would not share the results with the workers’ union or the author. After heated discussions, it agreed to share not the final report but individual test reports if each worker submitted an application in a self-addressed envelope. Only a few received their reports. The study’s overall findings were available only from the aggregate report filed by the NIOH in the Supreme Court in some other matter.
This case highlights the scant respect for ethically required practices such as ensuring privacy and providing information to the participants. These infringements violate not only the right to information on risks, but also the right to dignity. In a similar case, upon learning of the high incidence of silicosis among former workers in quartz crushing factories, the author visited some of their villages. A representation was made before the SHC, who agreed to investigate the matter. He asked the NIOH to carry out a study in coordination with the author and his colleagues. Accordingly, over 30 workers were examined at a camp. The workers waited for the results so that they could file compensation claims. However, the NIOH would not share the reports. It was only after petitioning the SHC that they were shared.
These cases provide just a glimpse of the vulnerability of workers while interacting with occupational health professionals and the system. A multipronged approach is necessary to address this problem. First, ethical guidelines should be adopted to facilitate the enforcement of legislations. The international codes and guidelines on ethics in occupational health and safety can be used as a template to develop India-specific guidelines. A national charter on ethical practice in occupational health can be developed in consultation with all the stakeholders, including occupational health experts, policy-makers, workers’ unions, factory owners and health activists. Institutionalisation of the guidelines by law is likely to promote ethical practice. It is only then that issues related to violations and malpractice can be raised, remedied and addressed.
Second, the legislations pertaining to workers’ health and safety must be better monitored and enforced. There is a need to revisit them and other policies to identify the gaps, understand the challenges in their implementation, plug the loopholes and bring them up to date with recent developments. It is equally important to allocate more resources, appoint staff where required and review the quality of the services provided to the workers. Third, to understand the occupational health burden in India, there must be transparency in data collection and the outcomes of studies conducted by agencies such as the NIOH should be shared. This will also help in planning and formulating strategies to address occupational health issues.
Conclusion
The government’s “Make in India” campaign is intended to transform the country into an industrial hub. Millions of workers, both in the organised and unorganised sectors, would form the backbone of this campaign. However, their health, safety and well-being are not accounted for in policy or practice. This paper focuses mainly on the fraction of organised workers who have managed to access the limited channels of occupational health services. The health needs of unorganised workers, who form the bulk of the labour force in the mining, manufacturing and construction sectors, have not been covered. These workers remain outside the purview of any law for the protection of their health and safety at work. The socalled “non-hazardous” service sectors, too, are associated with several occupational health problems which are not addressed by any law.
There is an urgent need to address these issues through deliberations with the stakeholders, modification of the existing laws and allocation of the required resources. Unless the relevant provisions are legally enforced, the barriers to OHS cannot be tackled. The laws should be framed on the basis of ethics. OHS laws can be enforced as part of the fundamental right to health and well-being only if they are underpinned by strong ethical codes and practical guidelines. It must be ensured that the laws are successful in identifying and addressing the challenges and gaps. Finally, it is important to take stock of policies, strategies and institutional frameworks that have succeeded in other countries and adapt these to the Indian context.
Declaration: The first author has been involved in activism and advocacy for the OSH rights of workers for the last 30 years.
This paper has not been funded by any organisation.
Notes
1A Lok Adalat, or “people’s court”, is a non-adversarial system of alternative dispute resolution and arbitration.
2Notified Occupational Diseases are those listed conditions that a medical doctor must report to the factory inspector of a unit if he comes across patients suffering from them.
3All cases and their locations have been anonymised.
References
- World Health Organization. Good practice in occupational health services: a contribution to workplace health. Copenhagen: WHO Regional office for Europe; 2002.
- International Commission on Occupational Health. International Code of Ethics For Occupational Health Professionals. Rome: ICOH, 2012.
- Simlai D. Work conditions in manufacturing industries of West Bengal. Management and Labour Studies. 2009;34(1):95-113. doi: 10.1177/0258042X0903400107.
- Das B. Assessment of occupational health problems and physiological stress among the brick field workers of West Bengal, India. Int J Occup Med Environ Health. 2014;27(3):413-25. doi: 10.2478/s13382-014-0262-z.
- International Labour Organization. Insights into working conditions in India’s garment industry/International Labour Office, Fundamental Principles and Rights at Work (Fundamentals). Geneva: ILO; 2015.
- Vikaspedia: Ministry of Communications and Information Technology. Unorganised labour force in India [Internet]. New Delhi: Ministry of Communications and Information Technology; 2012 [cited 2015 Dec 4]. Available from: http://vikaspedia.in/social-welfare/unorganisedsector-1/categories-of-unorganised-labour-force
- The Factories Act, 1948 (23rd September, 1948).
- Sood J. Farmers have decreased, farm labourers increased: census report, May 01, 20113 [Internet] [cited 2015 Dec 4]. Available from: http://www.downtoearth.org.in/news/farmers-have-decreased-farm-labourersincreased-census-report–40940
- International Labour Organization. Safety and health in agriculture. Geneva: ILO, 2011.
- Murlidhar V. An 11-year-old boy with silico-tuberculosis attributable to secondary exposure to sandstone mining in central India. BMJ Case Rep. 2015;2015. pii: bcr2015209315. doi: 10.1136/bcr-2015-209315.
- Patel J. A journey through 20 years of occupational health and safety in India. New Solut. 2014;23(4):643-54. doi: 10.2190/NS.23.4.g.
- Das S. Occupational fatalities in the construction sector: a medico-legal viewpoint. Med Leg J. 2015;83(2):93-7. doi: 10.1177/0025817214554869.
- International Labour Organization. Ratifications for India [Internet] [cited 2015 Dec 19]. Available from: http://www.ilo.org/dyn/normlex/en/f?p=1000:11200:0::NO:11200:P11200_COUNTRY_ID:102691
- International Labour Organization. International Labour Standards on Occupational Safety and Health [Internet] [cited 2015 Dec 19]. Available from: http://www.ilo.org/global/standards/subjects-covered-by-international-labour-standards/occupational-safety-and-health/lang–en/index.htm
- Ministry of Labour, Government of India. The Contract Labour (Regulation and Abolition Act); 1970 (September 5, 1970) [Internet] [cited 2016 Aug 30]. New Delhi: MoL;1970. Available from: http://labour.bih.nic.in/Acts/contract_labour_regulation_and_abolition_act_1970.pdf
- The Associated Chambers of Commerce of India. Rise of contract workers by 39% in 2013: ASSOCHAM. ASSOCHAM India; February 5, 2014.
- Karthyaeni V, Bhatt V. Lok adalats and permanent lok adalats in India [Internet] [cited 2015 Dec 27]. Available from: http://www.legalserviceindia.com/articles/lok_a.htm
- Takala J. Introductory report: decent work – safe work. Proceedings of the XVIth World Congress on Safety and Health at Work, Vienna, Germany, May 27, 2002. Geneva: ILO; 2002 [cited 2015 Dec 4]. Available from: http://www.ibram.org.br/sites/700/784/00001030.pdf
- Rao GS. India: The Report Of The Second Indian National Labour Commission-2002: an overview [Internet]. Mondaq, March 5, 2003 [cited 2015 Dec 4]. Available from: http://www.mondaq.com/india/x/20167/employee+rights+labour+relations/The+Report+Of+The+Second+Ind ian+National+Labour+Commission2002++An+Overview
- Ministry of Labour and Employment, Union of India. Employees’ State Insurance Act, 1948.New Delhi: MoLE; 1948 Apr 19. Available from: http://www.esic.nic.in/Tender/ESIAct1948Amendedupto010610.pdf
- Employees’ State Insurance Corporation. Annual Report 2013–14. New Delhi: ESIC; 2015.
- Vitthal Udyognagar Industries Association [Internet] [cited 2016 Jan 1]. Available from: http://www.vuia.org/about.php
- Asia Monitor Resource Centre. Invisible victims of development: workers health and safety in Asia. Hong Kong: Asia Monitor Resource Centre; 2012.
- Employees’ State Insurance Corporation .Press Release. 5th December 2014. http://esic.nic.in/press/Press_Release_05.12.14.pdf
- Dhobal H (editor). Writings on human rights, law and society in India – a combat law anthology. New Delhi: Human Rights Law Network; 2011.
- Concept paper on “Occupational safety and health” presented at the 5th India-EU Joint Seminar on Employment and Social Policy, New Delhi, September 19-20, 2011 [cited 2016 Jun 1]. Available from: https://toxicswatch.files.wordpress.com/2011/12/occupational-safety-andhealth-september-2011.pdf
- Ministry of Labour and Employment, Union of India. National Policy on Safety, Health and Environment at Workplace [Internet]. New Delhi: MoLE; 2009Feb [cited 2016 Jan 1]. Available from: http://dgfasli.nic.in/npolicy/OSH-Policy.pdf
- National Human Rights Commission. Special Report to Parliament of India on Silicosis, Aug 23, 2012 [cited 2016 Jan 1]. Available from: http://nhrc.nic.in/Documents/Reports/Special%20Report%20To%20Parliament%20of%20India%20On%20Silicosis.pdf
- Times of India. Rajasthan model to compensate ailing miners. Times of India, City Edition, Jaipur, May 22, 2014 [cited 2015 Dec 15]. Available from: http://timesofindia.indiatimes.com/city/jaipur/Rajasthan-model-to-compensate-ailing-miners/articleshow/35451250.cms
- Dhar A. Amend Mines Act to contain silicosis: State Human Rights Commission. The Hindu, April 5, 2015 [cited 2015 Dec 15]. Available from: http://www.thehindu.com/news/amend-mines-act-to-containsilicosis-state-human-rights-commission/article7070741.ece
- Economica India. Reports of the National Commission on Labour, 2002-1991-1967. Kolkata: Academic Foundation; 2003.
- Government of India. Report of the working group on Occupational safety and Health for the 12th Five-Year Plan (2012–2017). New Delhi: Ministry of Labour and Employment, Government of India, 2011 [cited 2016 Jun 1]. Available from: http://planningcommission.nic.in/aboutus/committee/wrkgrp12/wg_occup_safety.pdf
- London L, Tangwa G, Matchaba-Hove R, Mkhize N, Nwabueze R, Nyika A, Westerholm P. Ethics in occupational health: deliberations of an international workgroup addressing challenges in an African context. BMC Med Ethics. 2014;15:48. doi.10.1186/1472-6939-15-48.
- Directorate General, Factory Advice and Labour Institutes (DGFASLI). Statistics on Status of compliance with statutory provisions based on data collected by DGFASLI. Mumbai: DGFASLI; 2012.
- Director of Industrial Safety and Health, Government of Gujarat, Accidents [cited 2016 Jan 15]. Available from: http://dish.gujarat.gov.in/statistics-accidents.htm
- Lifelong Learning Programme-European Commission. Review and analysis of available accident statistics relating to lifting operations using rope access (Research and needs analysis) Part 2. Brussels: Education and Culture Director General-EC; 2013 [cited 2015 Jan 25]. Available from: http://www.adam-europe.eu/prj/8398/prd/2/4/WP2-Accident%20Report%20wrobb%20review%20SEP%2013T.pdf
- Westerholm P. The ethical challenges of the occupational physician in our time. G Ital Med Lav Ergon. 2010;32(4):403-6.
