ARTICLE
Selfless giving in medicine: a study of altruistic attitudes among medical students
Sanjai S, Vijayaprasad Gopichandran
Published online: September 19, 2017
DOI: https://doi.org/10.20529/IJME.2017.082
Abstract
Introduction: An important virtue in the medical profession is altruism, which makes a doctor serve without an excess of expectation of return.
Objectives: To assess the level of altruism and factors influencing altruism among medical students at a medical college in Chennai
Methods: A cross-sectional study was conducted on a sample of 224 students from the first, third and fourth years. We prepared a questionnaire which contained questions from the previously validated Altruistic Personality Scale. After the students’ informed consent was obtained, they were requested to self-administer the questionnaire in the form of a pen-and-paper test.
Results: The altruistic attitudes of the students were largely grouped into four categories on the basis of the factor analysis namely, (i) simple acts of altruism, (ii) recognised acts of charity, (iii) altruistic activities that put the self at risk, and (iv) humanitarian acts. From the factor scores obtained in this analysis, we performed a K-means cluster analysis, which showed that the students can be grouped into three clusters, namely, (i) simple altruists (43.3%), (ii) risk-taking altruists (30.8%), and (iii) limited altruists (25.9%). It was further observed that younger students, males, those whose parents donated to charity, those whose friends organised charitable group activities, and those who had role models in college were much more likely to be simple altruists.
Conclusion: Altruistic behaviours were infrequent among the sample of students studied, and such behaviours were influenced by their parents, peers and role models in college. An enabling environment should be created to nurture such tendencies and to channelise them through organised activities in medical schools.
Introduction
Altruistic acts are defined as acts of goodwill for the well-being of others, without any selfish intent (1). Altruism is exercised in several medical contexts, such as blood donation, organ donation and participation in clinical trials (1). It has been a primary virtue of medical practice over the years. Altruistic tendencies are implicit in the nature of a doctor (2). Doctors exhibit these tendencies by working towards the welfare of the patient beyond duty hours, sacrificing their break time for the sake of patients, providing treatment free of cost to the poor, risking their own lives to deliver services in zones of conflict and war, and risking their health to provide services during outbreaks of disease (3). In the past, doctors spent long hours taking care of patients in the hospital, without paying attention to their own families.
This behaviour was not questioned and, in fact, was accepted as a part of a doctor’s duty.
However, in recent years, increasing attention is being paid to the work–life balance of doctors and their work hours are being strictly regulated. It could be argued that such regulations have erased one of the primary expressions of the altruism implicit in the medical profession. With medicine assuming a consumer–provider model, the role of altruism becomes blurred.
Against this backdrop, it is challenging to explain the role of altruism and the role it plays in the delivery of medical care. It is no longer clear if altruism still plays an important role in medical care and whether such an attitude is sustainable in the present context. Certain scholars even propose that the term “altruism” is misleading in the medical context and should be replaced with “pro-social behaviours” (4, 5).
Mistrust in the medical profession has grown in recent years because of the increasing cases of medical malpractice and corruption. In this context, altruism may just be the remedy to salvage the level of trust patients have in the system. Before thinking of ways to improve altruism, it is important to understand whether an altruistic attitude exists among medical students in training, and if so, what its coordinates are. This study was conducted with the objective of assessing altruistic attitudes among medical students in a medical college in Chennai and determining the factors which influence altruism.
Methods
Study population
The study was conducted in a medical college in Chennai that is run by a social health insurance corporation. There were four batches of students enrolled in the MBBS course and each batch had permission to admit 100 students. Roughly 400 students were enrolled in the college at the time of the study. A majority of the seats (65%) were filled by students from the Tamil Nadu state medical college selection merit list. About 20% were filled by children of patients insured by the social health insurance scheme, while the remaining 15% were filled through the all-India medical entrance examination. The students predominantly belonged to the states of Tamil Nadu and Kerala, and some were from the northern states of India. All students were selected on the basis of academic merit and there were no capitation fees or donations for admission (additional payments beyond fees fixed by the government for admissions into medical school). The sampling for this study was done in a non-probabilistic manner. A total of 300 students were approached for the study since one batch (of 100 students) was on vacation. Whoever expressed willingness to participate was enrolled in the study. Thus, 300 students were considered eligible for the study and were approached; 224 of them participated in the study.
Study instrument
We developed a questionnaire which contained the Altruism Personality Scale items for measuring the degree of the altruistic tendency in students (6). The Altruism Personality Scale has 20 items on which respondents are required to rate the frequency with which they engage in certain altruistic behaviours. One of the limitations of the scale is that the frequency of the performance of an altruistic act can be captured only if the medical student m/has been exposed to that particular act. This holds good for almost all the items in the tool. If the respondents have never faced the situation, they will respond with “never”. Those who have not helped even when they have faced the situation will also answer “never”. Therefore, with respect to that act, the respondents obtain a low score if they have answered “never”, in the former case because one never knows how they would have reacted if they had faced the situation, and in the latter, because they reacted in a non-altruistic way. If it was, indeed, the former case, it can be compensated for by capturing the high levels of altruism that they displayed in other acts that they were exposed to. Two items which are not relevant in the Indian context were removed, namely, “I have helped a stranger’s car out of the snow,” and, “I have, before being asked, voluntarily looked after a neighbour’s pets or children without being paid for it.”
The study instrument also contained questions related to factors that influence altruism, such as parental influence, peer influence and the influence of role models in medical college. The final number of questions in the questionnaire was 30.
Data collection
The study topic was introduced to the students and informed consent was obtained from everybody who agreed to participate. The students were then handed the study questionnaire, which was to be answered using a pen and paper format. The data were entered in an MS Excel spreadsheet and analysed using SPSS Statistical Package version 21.
Statistical analysis
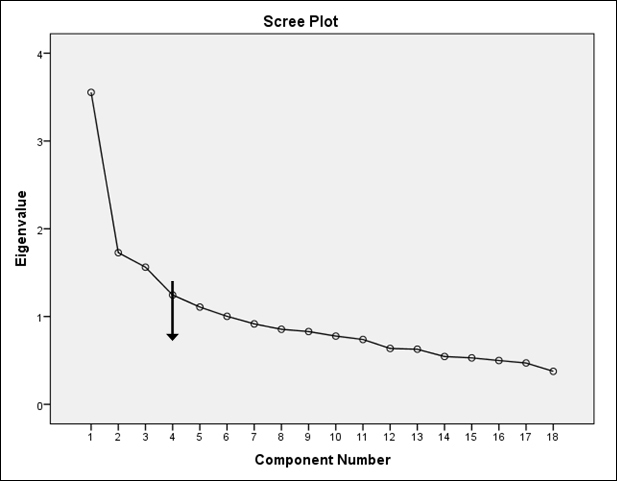
In order to recognise patterns in the data, one of the first steps is to reduce the dimensionality in the data. In this study, the main aim was to recognise patterns of altruism from the altruism behaviour frequency Likert data. There was a total of 18 items which had Likert scores. In order to better manage these 18 variables, they were first entered into a factor analysis model to reduce the dimensionality. The second step in the recognition of patterns is to cluster the data on the basis of common shared dimensions. To achieve this, k-means cluster analysis, which is a method of non-hierarchical partitioning, was performed. In the factor analysis, the required sample-to-variable ratio is 10:1 (7). Therefore, since the total number of variables entered into the model was 18, the required sample size was 180. A total of 224 samples were available for analysis, which made for an adequate sample-to-variable ratio. The responses to the items of the Altruistic Personality Scale were entered in an exploratory factor analysis, using principal component extraction, varimax rotation, both of which are statistical procedures used to reduce the number of questions to meaningful groups. The scree plot was used to decide on the number of factors to extract. On the basis of the factor scores obtained from the factor analysis, a hierarchical cluster analysis was performed to assess the optimal number of clusters into which the sample could be segmented. After this, k-means cluster analysis was performed. The sample was divided into three segments on the basis of this analysis. The characteristics of the students in each segment were analysed to understand the extent of altruism and the factors influencing altruism.
Ethical considerations
The study was approved by the institutional review board and ethics committee of the ESIC Medical College and PGIMSR, Chennai. Written informed consent was obtained from all the study participants. To maintain confidentiality, the participants were not required to enter their names in the questionnaires.
Results
Of a total of 300 students who were approached, 224 participated in the study, the response rate thus being 74.6%. Of the 224, 80 (35.7%) were first year students, 74 (33%) third year and 70 (31.3%) fourth year. The age range of the students was 17–23 years, with a median age of 19 years. Of the 224 participants, 147 (65.6%) were women. The characteristics of the study population are shown in Table 1.
| Table 1: Characteristics of the study population | |||
| S.No. | Character | Value | Frequency (%) |
| 1. | Year of study |
1 3 4 |
80 (35.7%) 74 (33%) 70 (31.3%) |
|
2. |
Age (in years) |
17 18 19 20 21 22 23 |
29 (12.9%) 35 (15.6%) 53 (23.7%) 43 (19.2%) 50 (22.3%) 12 (5.4%) 2 (0.9%) |
|
3. |
Gender |
Male Female |
77 (34.4%) 147 (65.6%) |
|
4. |
Native place |
City Town Village |
83 (37.1%) 80 (35.7%) 59 (26.3%) |
|
5. |
Type of school |
Private State |
170 (75.9%) 49 (21.9%) |
|
6. |
Religion |
Hindu Muslim Christian |
184 (82.1%) 11 (4.9%) 26 (11.6%) |
The responses of the students to the items in the Altruistic Personality Scale are shown in Table 2. It may be seen that simple acts, such as “giving directions to strangers”, “giving change to strangers”, “donating to charity”, “helping to carry a stranger’s things” and “holding the elevator doors open for a stranger”, were more frequent than acts such as “giving money to strangers”, “donating blood” and “giving a lift to a stranger in a car”. Overall, the frequency of most altruistic behaviours was reported as “never”, “once” or “more than once”.
| Table 2: Altruistic personality scale responses | |||||||
| S.No. | Questions | Responses | |||||
| Never | Once | More than once | Often | Very often | |||
| 1. | I have helped push a stranger’s car that was broken down or out of petrol.* | 147 (65.6%) | 37 (16.5%) | 32 (14.3%) | 3 (1.3%) | 3 (1.3%) | |
| 2. | I have given directions to a stranger. | 2 (0.9%) | 13 (5.8%) | 103 (46%) | 72 (32.1%) | 34 (15.2%) | |
| 3. | I have given change to a stranger.* | 62 (27.7%) | 40 (17.9%) | 91 (40.6%) | 23 (10.3%) | 7 (3.1%) | |
| 4. | I have given money to a charity.* | 23 (10.3%) | 32 (14.3%) | 99 (44.2%) | 37 (16.5%) | 32 (14.3%) | |
| 5. | I have given money to a stranger who needed it (or asked me for it). | 69 (30.8%) | 52 (23.2%) | 75 (33.5%) | 19 (8.5%) | 9 (4%) | |
| 6. | I have donated goods or clothes to a charity. | 14 (6.3%) | 42 (18.8%) | 84 (37.5%) | 48 (21.4%) | 36 (16.1%) | |
| 7. | I have done volunteer work for a charity. | 115 (51.3%) | 50 (22.3%) | 41 (18.3%) | 14 (6.3%) | 4 (1.8%) | |
| 8. | I have donated blood. | 182 (81.3%) | 27 (12.1) | 9 (4%) | 4 (1.8%) | 2 (0.9%) | |
| 9. | I have helped carry a stranger’s belongings (books, parcels, etc.).* | 61 (27.2%) | 47 (21%) | 75 (33.5%) | 23 (10.3%) | 17 (7.6%) | |
| 10. | I have delayed a lift and held the door open for a stranger.* | 73 (32.6%) | 28 (12.5%) | 61 (27.2%) | 45 (20.1%) | 16 (7.1%) | |
| 11. | I have allowed someone to go ahead of me in a line (in the supermarket, at a fast food restaurant). | 34 (15.2%) | 27 (12.1%) | 95 (42.4%) | 46 (20.5%) | 22 (9.8%) | |
| 12. | I have given a stranger a lift in my car.* | 169 (75.4%) | 22 (9.8%) | 21 (9.4%) | 10 (4.5%) | 1 (0.4%) | |
| 13. | l have pointed out a clerk’s error (in a bank, at the supermarket) when he has given more money for an item instead of the correct change.* | 36 (16.1%) | 38 (17%) | 96 (42.9%) | 30 (13.4%) | 22 (9.8%) | |
| 14. | I have let a neighbour whom I didn’t know too well borrow an item of some value to me (eg a dish, tools, etc.) | 70 (31.3%) | 42 (18.8%) | 68 (30.4%) | 31 (13.8%) | 13 (5.8%) | |
| 15. | I have helped a classmate whom I did not know that well with an assignment when my knowledge was greater than his or hers.* | 18 (8%) | 35 (15.6%) | 81 (36.2%) | 47 (21%) | 41 (18.3%) | |
| 16. | I have offered to help a handicapped or elderly stranger across a street. | 45 (20.1%) | 54 (24.1%) | 82 (36.6%) | 30 (13.4%) | 13 (5.8%) | |
| 17. | I have offered my seat on a bus or train to a stranger without a seat. | 27 (12.1%) | 38 (17%) | 86 (38.4%) | 53 (23.7%) | 20 (8.9%) | |
| 18. | I have helped a friend move into another house.* | 75 (33.5%) | 49 (21.9%) | 57 (25.4%) | 30 (13.4%) | 12 (5.4%) | |
| *Because of missing responses, the numbers do not add up to 224. | |||||||
With respect to factors influencing altruism, 87% of the respondents mentioned that their parents often donated to charity and 86% agreed that they learnt altruism from their parents. Only about 15% mentioned that their friends frequently organised charitable events and donations. About 25% of the students had role models in college and about 63% mentioned that their role models were altruistic.
Factor analysis of the 18 items in the Altruistic Personality Scale brought out extraction of four factors which explained 45% of the total variance. All items with factor loadings of less than 0.4 were excluded from the analysis. The KMO measure of sampling adequacy was 0.736, indicating an acceptable sample size, and the Bartlett’s test of sphericity showed a p<0.001, indicating a fit of the factor model. Four factors were extracted on the basis of the scree plot shown in Figure 1. The four factors, representing groups of altruistic behaviours, included simple acts of altruism, recognised acts of charity, greater acts of altruism and humanitarian acts. Two items, namely “I have given directions to a stranger” and “I have delayed a lift and held the door open for a stranger”, were removed from the analysis as the factor loadings were below 0.4. One item, namely “I have helped a classmate who I did not know that well with an assignment when my knowledge was greater than his or hers”, was removed because it had a very high degree of intercorrelation with other items in the factor. The items that loaded in the four factors and their factor loadings are shown in Table 3.
| Table 3: Factors extracted from the altruistic personality scale and their factor loading | ||
| S.No. | Item | Factor loading |
| Factor 1 – Simple acts of altruism | ||
| 1. | I have given change to a stranger. | 0.608 |
| 2. | I have allowed someone to go ahead of me in a line (in the supermarket, at a fast food restaurant). | 0.603 |
| 3. | I have let a neighbour whom I didn’t know too well borrow an item of some value to me (eg a dish, tools, etc.). | 0.555 |
| 4. | l have pointed out a clerk’s error (in a bank, at the supermarket) when he has given more money for an item instead of correct change. | 0.490 |
| 5. | I have given money to a stranger who needed it (or asked me for it). | 0.478 |
| 6. | I have helped carry a stranger’s belongings (books, parcels, etc.). | 0.466 |
| Factor 2 – Recognised acts of charity | ||
| 7. | I have donated goods or clothes to a charity. | 0.746 |
| 8. | I have done volunteer work for a charity. | 0.693 |
| 9. | I have given money to a charity. | 0.631 |
| Factor 3 – Greater acts of altruism | ||
| 10. | I have helped push a stranger’s car that was broken down or out of petrol. | 0.689 |
| 11. | I have donated blood. | 0.597 |
| 12. | I have given a stranger a lift in my car. | 0.567 |
| 13. | I have helped a friend to move to another house. | 0.463 |
| Factor 4 – Humanitarian acts | ||
| 14. | I have offered my seat on a bus or train to a stranger without a seat. | 0.683 |
| 15. | I have offered to help a handicapped or elderly stranger across a street. | 0.644 |
Hierarchical cluster analysis using the factor scores revealed that the sample could be optimally divided into three clusters.
It is seen that Cluster 1 (simple altruists) includes students who perform recognised acts of charity, simple acts of altruism and humanitarian acts, but score negatively in greater acts of altruism. Cluster 2 (risk-taking altruists) consists of students who predominantly perform greater acts of altruism and simple acts of altruism, but score negatively in recognised charitable activities and humanitarian acts. The final cluster, Cluster 3 (limited altruists), comprises students who score high in humanitarian acts, but negatively in all other acts of altruism.
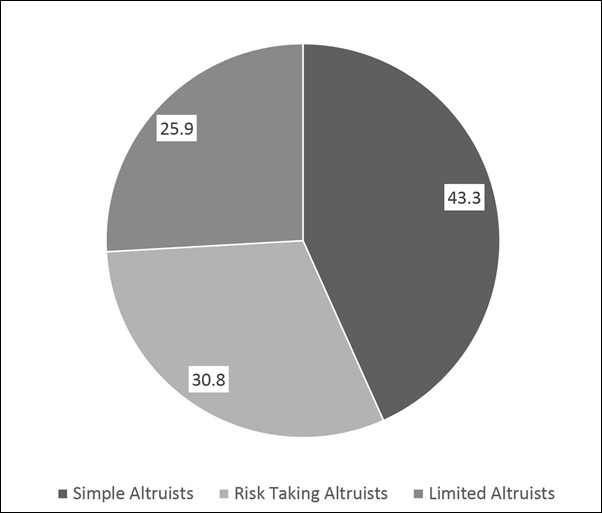
Figure 2 shows the prevalence of different types of altruists among the students. It may be observed that about 43% are simple altruists, 31% risk-taking altruists and about 26% limited altruists. This means that about 43% of the students perform simple acts of altruism, such as donating to charity, about 31% perform risky acts of altruism, such as blood donation and pushing a stranger’s broken down car, and 26% are limited altruists who confine themselves to basic humanitarian acts, such as offering their seat in a bus to another passenger.
It is probably a good sign if the medical students belong to the cluster of simple altruists or risk-taking altruists since it indicates an altruistic attitude. However, it is a poor sign if they belong to the group of limited altruists, as this indicates that their altruistic attitude is very limited. The influence of parental altruism, peer altruism and role modelling on the altruistic behaviours of the students is shown in Table 4. More of those students whose parents frequently donated to charity belonged to the group of simple altruists. Students whose friends frequently organised altruistic and charitable events also predominantly belonged to this group. Moreover, it was the students in this group who reported that they learnt their altruistic behaviour from their role models. The table indicates that with increasing age, the students increasingly became limited altruists. It was seen that more male respondents than females were risk-taking altruists and more female respondents were simple altruists. No other demographic factor, such as native place, type of school attended or religion, had a significant influence on the respondents’ nature of altruism.
| Table 4: Factors influencing medical students’ altruistic behaviours | ||||||
| S.No. | Factor | Categories | Cluster | p value | ||
| Simple altruists | Risk-taking altruists | Limited altruists | ||||
| 1. | Year of Study |
1 3 4 |
38 (47.5%) 31 (41.9%) 28 (40.0%) |
23 (28.8%) 25 (33.8%) 21 (30.0%) |
19 (23.8%) 18 (24.3%) 21 (30.0%) |
0.819 |
| 2. | Age (years) |
17 18 1 9 20 21 22 23 |
15 (51.7%) 15 (42.9%) 27 (50.9%) 17 (39.5%) 21 (42.0%) 21 (6.7%) 0 (0.0%) |
6 (20.7%) 1
2 (34.3%) 15 (28.3%) 12 (27.9%) 21 (42.0%) 3 (25.0%) 0 (0.0%) |
8 (27.6%)
8 (22.9%) 11 (20.8%) 14 (32.6%) 8 (16.0%) 7 (58.3%) 2 (100.0%) |
0.054* |
| 3. | Gender |
M F |
12 (15.6%) 85 (57.8%) |
48 (62.3%) 21 (14.3%) |
17 (22.1%) 41 (27.9%) |
<0.001*** |
| 4. | My parents donate to charity. |
Never Once More than once Often Very often |
3 (27.30%) 4 (22.20%) 22 (35.50%) 24 (35.80%) 44 (66.70%) |
6 (54.50%) 9 (50.00%) 20 (32.30%) 19 (28.40%) 15 (22.70%) |
2 (18.20%) 5 (27.80%) 20 (32.30%) 24 (35.80%) 7 (10.60%) |
<0.001*** |
| 5. | Some of my close friends, as a group, organise charitable activities in which I participate. |
Never Once More than once Often Very often |
33 (36.30%) 26 (44.80%) 13 (36.10%) 19 (67.90%) 5 (83.30%) |
31 (34.10%) 19 (32.80%) 13 (36.10%) 5 (17.90%) 1 (16.70%) |
27 (29.70%) 13 (22.40%) 10 (27.80%) 4 (14.30%) 0 (0.00%) |
0.016** |
| 6. | I learned to donate or give to other people from my role model. |
Strongly disagree Disagree N-A-N-DA Agree Strongly agree |
15 (23.80%) 7 (35.00%) 16 (55.20%) 32 (50.00%) 25 (55.60%) |
23 (36.50%) 8 (40.00%) 8 (27.60%) 16 (25.00%) 13 (28.90%) |
25 (39.70%) 5 (25.00%) 5 (17.20%) 16 (25.00%) 7 (15.60%) |
0.033** |
| *Indicative/not significant; **p<0.05; ***p<0.001; N-A-N-DA – neither agree nor disagree | ||||||
Discussion
While traditional medical practice has relied largely on altruism as a professional value, recent years have seen a shift in focus from “altruism” to “pro-social behaviours” (4, 5, 8). The main reason for this shift has been the idea that altruism is difficult to sustain despite several measures of reciprocity. However, most literature on altruism in the medical profession originates in the West. Researchers from the UK have commented that understanding the extent of altruism and its overall decline among medical professionals is essential for planning of the healthcare workforce (9). In contrast, scholars from the USA hold that in healthcare, “beneficence” is a more appropriate value than altruism (10). Certain other scholars use the word supererogation, and not altruism, to describe doctors who go beyond their call of duty and work beyond their duty hours, and hold that supererogation is not a necessary trait of medical professionalism (11). Hardly much has been understood about the altruistic motivations of medical students and medical professionals in the Indian context.
In this study, an attempt was made to quantify altruism among medical students in a medical college in Chennai. The previously validated altruistic personality scale did not mention any medical scenarios and was not specific to the practice of medicine. It attempted to capture the general altruistic attitudes of the students. This study found that the frequency of altruistic behaviours among the medical students was low. Of those who showed altruistic behaviour, about 43% emerged as simple altruists. The study also found that with increasing age, the extent of altruism declined. Before delving into a detailed discussion of the implications of this study, it would be useful to describe the way the various types of altruism were defined for the purpose of this study. It is noteworthy that these definitions were not provided by the original developers of the scale. We developed the definitions for the sake of clarity. Simple altruism was defined as acts of altruism which do not involve any relatively high level of risk to the self, physical, mental, social or emotional. Some examples are giving someone directions to a place and giving a person one’s place in a queue. Risk-taking altruism was defined as acts of altruism which entail a higher level of risk to the self, for example, pushing someone’s car and donating blood. Finally, limited altruism was defined as those acts which are a matter of basic etiquette and not specifically considered unique acts of altruism, such as offering one’s seat in the bus to an elderly woman.
Women were more likely to be simple altruists than men, who were more likely to be risk-taking altruists. Previous studies in the West have shown that expensive altruistic behaviours (eg donating expensive goods) are more common among women and inexpensive altruistic behaviours are more common among men. Men are more likely to be “all or none” type of altruists, whereas women tend to be more egalitarian in their approach (12). In our study, simple altruistic behaviour was influenced by the altruistic tendencies of the parents, peers and role models. The findings of this study have important implications for the education of medical students in medical professionalism.
Medical altruism and moral obligation to do good
Medicine is one of the few professions which is supposed to be dominated by unselfish motives. However, this dimension of medical practice may be a misrepresentation, as the doctor’s duty to put the patient’s interest ahead of his/her own is fiduciary in nature. It is a moral obligation and not something done out of the “goodness of one’s heart”. Therefore, what a doctor routinely does is not altruistic in the true sense of the word (10). However, this does not preclude the analysis of altruism as a virtue in the practice of medicine. Altruism among doctors, though not an obligatory professional virtue, may play a role in shaping the typical characteristics of the doctor–patient relationship. Altruism entails going beyond the call of duty and helps to build trusting doctor–patient relationships. It is not feasible to make altruism a moral obligation in the practice of medicine. However, it may be important to promote altruistic tendencies among doctors as a virtue worth possessing.
What influences medical altruism?
Among the earliest influences on child behaviour are the attitudes and behaviours of the parents. Therefore, parental behaviours have a strong influence on children. Studies have shown that parental and environmental influences have a significant role in promoting pro-social behaviours among children (13). Our study found that parental role modelling had a significant influence on the altruistic tendencies of children. The influence was limited to simple altruistic acts, such as giving change to a stranger and allowing somebody to pass ahead in a queue, which do not expose the individual to much risk. Simple altruistic behaviours were also influenced by charitable events organised and conducted by peers, and by role models in college. Parental influence was not present among students who were risk-taking altruists. This probably implies that risk-taking altruism, including activities such as donating blood and giving somebody a lift in one’s car, is not a learned attribute.
As the students progressed through medical college, their altruistic behaviours became less frequent. This can probably be attributed to several situations which test their character – an increasing workload, an inability to deal with the demands of the curriculum, and the influence of teachers who are, in turn, pressed by market forces. It is likely that the students’ altruistic behaviours are compromised as a means of self-preservation.
While interpreting the factors which influence altruism among medical students, it is also important to consider the traditional social values that have informed human behaviours in India and the changes in these values in recent times. The Gandhian principle of altruistic individualism was the mainstay of moral values in Indian society. Altruistic individualism is an “other-centred” individualism, as opposed to the “self-centred” individualism that is popular in western cultures (14). However, Indian society has been witnessing a gradual change in this value, and this may have its own influence on the altruistic attitudes of medical students.
Altruism as an aspect of medical professionalism
Epstein and Hundert have defined medical professionalism as “the habitual and judicious use of communication, knowledge, technical skills, clinical reasoning, emotions, values, and reflection in daily practice for the benefit of the individual and community being served” (15). One other definition of medical professionalism is “behaviours by which physicians demonstrate that they are worthy of the trust that is bestowed upon them by patients and the public because they work for the patients’ and public’s good”. Some of the important aspects of professionalism thus defined are placing self-interest below the interest of patients; adhering to high moral standards; investing in core humanistic values, such as honesty, integrity, compassion, altruism, respect, commitment to excellence, accountability and a reflective mindset; and an ability to deal with complexity and uncertainty (16). Therefore, though altruism cannot be termed a fiduciary duty of the doctor, it can be perceived as a professional virtue that the doctor should strive to achieve. Further, medical altruism could be the remedy for the health system, which is suffering from a serious erosion of trust (17).
Implications for curriculum for medical professionalism
The curriculum for medical professionalism, apart from helping students prepare for a career of lifelong self-learning and strive for excellence in their profession, should also emphasise skills such as communication, empathy, emotional intelligence and professional values. Altruism has been an important value in medicine from the olden days. As shown by this study, parents, peers and role models can significantly influence most of the students’ altruistic tendencies. In addition to these influences, the curriculum for education in professional values should include organised altruistic acts, such as voluntary activities, participation in medical camps and humanitarian activities. It is argued that this could motivate students to develop and enhance their altruistic tendencies, which, in turn, would improve their levels of professionalism and help to bring about valuable changes in the healthcare system.
Conflicts of Interest
None declared
Declaration
This paper was presented as an oral paper at the sixth National Bioethics Conference held in Pune in January 2017.
References
- Steinberg D. Altruism in medicine: its definition, nature, and dilemmas. Cambridge Q Healthc Ethics. Cambridge Univ Press; 2010;19(2):249-57.
- Saks M. Professions and the public interest: Medical power, altruism and alternative medicine. Routledge; 2005.
- Jones R. Declining altruism in medicine. BMJ. 2002;324(7338):624-5.
- Bishop JP, Rees CE. Hero or has-been: is there a future for altruism in medical education? Adv Health Sci Educ Theory Pract. 2007;12(3):391-9.
- Burks DJ, Kobus AM. The legacy of altruism in health care: the promotion of empathy, prosociality and humanism. Med Educ. 2012 Mar;46(3):317-25. doi: 10.1111/j.1365-2923.2011.04159.x.
- Rushton JP, Chrisjohn RD, Fekken GC. The altruistic personality and the self-report altruism scale. Pers Individ Differ. 1981;2(4):293-302. DOI: 10.1016/0191-8869(81)90084-2.
- Barrett PT, Kline P. The observation to variable ratio in factor analysis. Personality Study & Group Behaviour.1981;1(1):23-33.
- Pilowsky I. Altruism and the practice of medicine. Br J Med Psychol. 1977;50(4):305-11.
- Jones R. Declining altruism in medicine; understanding medical altruism is important in workforce planning. BMJ. 2002 Mar 16; 324(7338):624-5.
- Glannon W, Ross LF. Are doctors altruistic? J Med Ethics. 2002 Apr 1 [cited 2017 Aug 25];28(2):68-9. Available from: http://jme.bmj.com/content/28/2/68.abstract
- Downie RS. Supererogation and altruism: a comment. J Med Ethics. 2002;28(2):75-6.
- Andreoni J, Vesterlund L. Which is the fair sex? Gender differences in altruism*. Q J Econ [Internet]. 2001 Feb 1 [cited 2017 Aug 25];116(1):293-312. Available from: http://dx.doi.org/10.1162/003355301556419
- Knafo A, Plomin R. Prosocial behavior from early to middle childhood: genetic and environmental influences on stability and change. Dev Psychol. 2006 Sep;42(5):771-86.
- Madan TN. Gandhi’s altruistic individualism. The Hindu [Internet]. Chennai; 2002 Oct 2 [cited 2017 Aug 25]. Available from: http://www.thehindu.com/2002/10/02/stories/2002100200031000.htm
- Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002 Jan 9;287(2):226-35.
- Swick HM. Toward a normative definition of medical professionalism. Acad Med. 2000 Jun;75(6):612-6.
- Kane S, Calnan M. Erosion of trust in the medical profession in India: time for doctors to act. Int J Health Policy Manag. 2016 Nov 2 [cited 2017 Aug 25];6(1):5-8. doi: 10.15171/ijhpm.2016.143. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5193507/
